Office billing
Here is a typical but very simple example of how a medical office bills for services based on the regulations imposed.
We’ll take the example of a 65 y.o. female who comes to the office complaining of 2 days of fever and burning on urination.
She is taken back to the exam room where her blood pressure, pulse, respirations and temperature are obtained.
She is examined and questioned by the doctor who then orders a complete blood count (CBC) and a urinalysis (U/A).
After he reviews the results and talks more with the patient, he writes a prescription for an antibiotic and she checks out of the office.
The billing process involves filing the claim on a specialized form called a HCFA 1500. (See image)
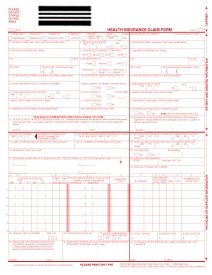
Every procedure that is to be billed has to have a specific code (CPT code) filed on the form. In addition, every procedure (CPT code) has to be associated with an acceptable diagnosis code (ICD-9 code).
If a CPT code is associated with an ICD-9 code that isn’t approved as an acceptable diagnosis for that test or procedure, the claim will be rejected. (Medicare and insurance companies decide if the code you are using justifies what was ordered)
So for the example above, the following information has to be sent with everything in their correct boxes on the form. If something is missing, the claim is rejected.
A routine Office visit has a CPT code of 99213 and corresponds with the diagnosis of UTI that has an ICD-9 code of 599.0
A CBC has a CPT code of 85025 and is linked with the diagnosis of fever that has an ICD-9 code of 780.6
The U/A has a CPT code of 81002 and is linked to the diagnosis of UTI that has an ICD-9 code of 599.0
Since this is a Medicare patient and we do accept assignment, the following would be charged and collected if everything is perfect.
Procedure 99213 (office visit) has an office charge of $70. Medicare only allows $49.79 and only pays 80% which is $39.83. The leaves the patient responsible for $10.07.
The 85025 (CBC) has an office charge of $35. Medicare only allows $10.86 and only pays $8.68 leaving the patient responsible for $2.18.
The 81002 (U/A) has an office charge of $10. Medicare only allows $3.57 and only pays $2.86 leaving the patient responsible for $0.71
So for the example above, if every “I” is dotted and every “t” crossed, and all codes match and the claim is not rejected, the total billed to Medicare is $115.
Medicare says the visit is only worth $64.22 and out of that they are only paying $51.37.
The patient will then be billed for the remainder of $13.96
If anything is rejected, the claim has to be refiled. The patient has to be billed for the remainder and each one of these claims has to be tracked and followed up on if they are not paid.
This claim is simple. But when there are several diagnoses and procedures it becomes much more complicated. Some patients may have Diabetes, Hypertension, Heart Disease, thyroid problems and may get 4 or 5 different lab tests or other procedures done. The process can get very complicated and the codes can be very similar; all contributing to possible errors.
Private insurance companies may have their own set of rules and billing guidelines. They are always eager to deny claims for any trivial reason. We will discuss some other problems in the billing cycle in the coming days.
We’ll take the example of a 65 y.o. female who comes to the office complaining of 2 days of fever and burning on urination.
She is taken back to the exam room where her blood pressure, pulse, respirations and temperature are obtained.
She is examined and questioned by the doctor who then orders a complete blood count (CBC) and a urinalysis (U/A).
After he reviews the results and talks more with the patient, he writes a prescription for an antibiotic and she checks out of the office.
The billing process involves filing the claim on a specialized form called a HCFA 1500. (See image)
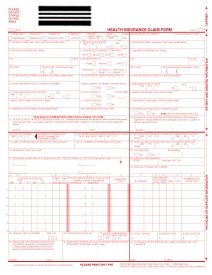
Every procedure that is to be billed has to have a specific code (CPT code) filed on the form. In addition, every procedure (CPT code) has to be associated with an acceptable diagnosis code (ICD-9 code).
If a CPT code is associated with an ICD-9 code that isn’t approved as an acceptable diagnosis for that test or procedure, the claim will be rejected. (Medicare and insurance companies decide if the code you are using justifies what was ordered)
So for the example above, the following information has to be sent with everything in their correct boxes on the form. If something is missing, the claim is rejected.
A routine Office visit has a CPT code of 99213 and corresponds with the diagnosis of UTI that has an ICD-9 code of 599.0
A CBC has a CPT code of 85025 and is linked with the diagnosis of fever that has an ICD-9 code of 780.6
The U/A has a CPT code of 81002 and is linked to the diagnosis of UTI that has an ICD-9 code of 599.0
Since this is a Medicare patient and we do accept assignment, the following would be charged and collected if everything is perfect.
Procedure 99213 (office visit) has an office charge of $70. Medicare only allows $49.79 and only pays 80% which is $39.83. The leaves the patient responsible for $10.07.
The 85025 (CBC) has an office charge of $35. Medicare only allows $10.86 and only pays $8.68 leaving the patient responsible for $2.18.
The 81002 (U/A) has an office charge of $10. Medicare only allows $3.57 and only pays $2.86 leaving the patient responsible for $0.71
So for the example above, if every “I” is dotted and every “t” crossed, and all codes match and the claim is not rejected, the total billed to Medicare is $115.
Medicare says the visit is only worth $64.22 and out of that they are only paying $51.37.
The patient will then be billed for the remainder of $13.96
If anything is rejected, the claim has to be refiled. The patient has to be billed for the remainder and each one of these claims has to be tracked and followed up on if they are not paid.
This claim is simple. But when there are several diagnoses and procedures it becomes much more complicated. Some patients may have Diabetes, Hypertension, Heart Disease, thyroid problems and may get 4 or 5 different lab tests or other procedures done. The process can get very complicated and the codes can be very similar; all contributing to possible errors.
Private insurance companies may have their own set of rules and billing guidelines. They are always eager to deny claims for any trivial reason. We will discuss some other problems in the billing cycle in the coming days.

0 Comments:
Post a Comment
<< Home